Sachar Dental NYC
For SAME day / emergency appointments
Call (212) 752-1163
All the below content has been written by NYC Dentist, Dr. Sandip Sachar.
Dentist NYC -What is Periodontal Disease
On this page: (Click topic below)
What is periodontal disease (aka gum disease)?
What causes periodontal disease?
What are the signs and symptoms of periodontal disease?
How can I prevent gum disease?
How is a periodontal disease diagnosed?
How is periodontal disease treated?
Why are we the best dentists in NYC for periodontal disease?
Periodontal Disease
What is periodontal disease (aka gum disease)?
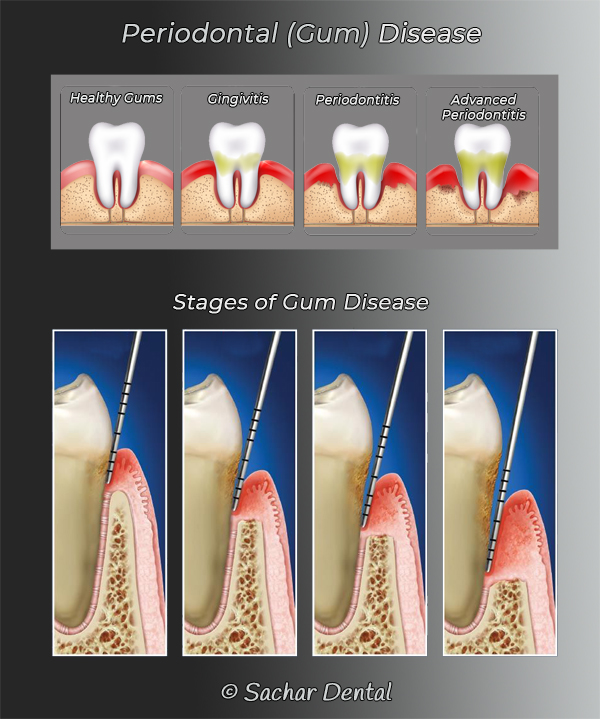
Another name for periodontal disease is gum disease. Periodontal disease is a progressive disease that starts with mild inflammation of the gums, called gingivitis. It can worsen and eventually lead to loss of the teeth, and loss of bone. Most often, it is caused by bacteria, tartar and plaque that build up in and around the teeth and gums.
What causes periodontal disease?
Most often, the cause of periodontal disease is the accumulation of bacteria, tartar and plaque in, and around the teeth and gums. This occurs when one does not perform proper oral hygiene. Proper oral hygiene involves flossing and brushing daily at home, as well as coming into our office at least twice per year for professional dental cleanings and checkups.
When plaque and tartar accumulate on the teeth and under the gums, bacteria use them as a source of nourishment, or medium to live off of. When bacteria accumulate, they release destructive enzymes and acids that slowly destroy the gums and the jawbone where the teeth attach. When this bone loss occurs, teeth may get loose and eventually fall out. Periodontal disease is the leading cause of tooth loss in the USA.
What are the signs and symptoms of periodontal disease?
Pain is rarely present in periodontal disease. It is sometimes asymptomatic, however, it may include the following list of possible symptoms:
- Bleeding gums
- Sore gums
- Loose teeth
- Tooth sensitivity
- Gum recession (shrinking gums with increased tooth root exposure)
- Bad breath
- Swollen gums
- Change in the tooth alignment
How can I prevent gum disease?
Gum disease can be easily prevented with proper oral care at home, such as brushing and flossing. Professional dental cleanings twice (or more times) per year are also very important to prevent gum disease.
Important terminology regarding periodontal disease.
The following is a list and description of terms that one may hear when discussing periodontal disease. In no particular order, it is important to understand the following terminology:
Tartar – Tartar is found between the teeth, on the teeth, and sometimes under the gums. It consists of food particles that have hardened over time and become adhered to the surface of the teeth. It also contains bacteria that can cause inflammation of the gums. Unfortunately, tartar cannot be removed with a toothbrush nor floss alone. Once the food particles have hardened, it requires a professional dental cleaning to remove them. Left alone and untreated, tartar and bacteria can lead to extensive periodontal disease.
Calculus - Calculus is another name for Tartar.
Plaque – Plaque is found between the teeth, on the teeth, and sometimes under the gums as well. It consists of food particles and bacteria. Left alone, plaque will eventually harden into tartar. Plaque can be removed by flossing and brushing regularly. However, it often accumulates in areas that are hard to get to with floss or a toothbrush. Plaque that is left after flossing and brushing will be removed during your professional dental cleanings. Over time, accumulation of plaque can lead to tooth decay, gum inflammation and periodontal disease.
Gingivitis – Gingivitis is the first stage of periodontal disease. It is another term for inflammation of the gums. The gums can get inflamed due to the accumulation of bacteria, plaque and tartar. With gingivitis, one may notice bleeding of the gums while brushing and flossing. Under normal circumstances, healthy gums do not bleed when flossing and brushing. Bleeding gums is a common symptom seen at the start of periodontal disease, or gingivitis. When treated during this early stage of periodontal disease, a professional dental cleaning can stop the progression of periodontal disease and be reversed.
Periodontitis – Periodontitis is another name for infection of the gums and the jaw bone. Periodontitis occurs when bacteria penetrate deep under the gums and start to erode the bone where the teeth attach to it. It is considered normal to have a gum pocket depth of 3 mm or less. When there exists gum pockets that are deeper than 3 mm, it is considered periodontal disease. In the early stages, this may be treated with a deep cleaning. Periodontitis is the leading cause of tooth loss. A deep cleaning may be able to prevent erosion of bone and eventual loss of teeth. In most cases, periodontitis may be pain-free and not noticed. Therefore, it is very important to have regular dental checkups to catch it early and professional cleanings to prevent it.
Gum pockets – The space between the root of the tooth and the gums is called the gum pocket. Normally, it is no deeper than 3 mm in healthy gums. When bacteria get inside a gum pocket, and they become deeper than 3 mm, it is considered periodontal disease. This allows bacteria to accumulate under the gums that cannot be removed with brushing and flossing alone. Left untreated, bacteria within the gum pockets can erode the bone and progress to worsen periodontal disease.
Dental Cleaning – A dental cleaning is a procedure that is performed by a dental hygienist or dentist in order to remove plaque, tartar and bacteria from on the teeth as well as between them and below the gums. It is recommended by the American Dental Association (ADA) to have a professional dental cleaning at least twice per year. It is often done with an ultrasonic, high-pressure water jet scaler or by hands, manually with a hand scaler. It is a superficial cleaning of the teeth and gums that does not penetrate more than 3 mm into the gum pockets.
Prophylaxis - Prophylaxis is another word for dental cleaning. A cleaning is a prevention to prevent gum diseases and tooth decay.
Deep Cleaning – A deep cleaning is a professional dental cleaning that is performed when the gum pockets are found to be deeper than 3 mm. The gum pockets are the space between the root of the tooth and the gums where bacteria, plaque and tartar can accumulate. When deeper than 3 mm, it is hard to remove them with flossing and brushing alone. It then requires a professional deep cleaning. A deep cleaning is very similar to a regular professional dental cleaning, however, it requires anesthesia to allow the dentists to clean deeper within the gums. This also allows the patient to be comfortable and not have pain during a deep cleaning. We are able to remove plaque, tartar and bacteria from deep within the root of the teeth and under the gums.
Scaler – A scaler is another name for the dental instrument that is utilized to remove plaque, tartar and bacteria from the teeth, between them, as well as under the gums. A scaler can be a metallic hand instrument for manual scaling, or be an ultrasonic, high-pressure water jet.
Cavitron – A Cavitron is a dental device that is used by dental hygienist and dentists to perform teeth cleaning. It uses high-pressure water and ultrasound to remove plaque, tartar and bacteria from the teeth, between them, as well as under the gums. It is able to gently flush under the gums to provide an efficient and pain-free cleaning.
Prophy paste - Prophy paste is the polishing powder that is utilized to remove staining from the teeth. It is applied with a high-speed spinning brush.
How is a periodontal disease diagnosed?
Periodontal disease is diagnosed through a clinical examination and with x-rays. Through an examination, our dentists will identify when there exists gingivitis, deep gum pockets and bone erosion all associated with periodontal disease. It is important to have dental checkups at least twice per year in order to catch periodontal disease before it progresses. When caught early, periodontal disease is much more treatable than when it advances into the later and more destructive stages.
How is periodontal disease treated?
In the very early stages, periodontal disease may be treated with a professional dental cleaning to remove all tartar, plaque and bacteria from the teeth, around them, and under the gums. When periodontal disease advances slightly, a deep cleaning may be able to treat periodontal disease and prevent it from getting worse. A deep cleaning is performed when the gum pockets are greater than 3 mm deep. A deep cleaning involves anesthesia to enable deeper cleaning to be comfortable for the patient. After having a deep cleaning, we often recommend that our patients have regular professional dental cleanings four times per year instead of twice per year.
When periodontal disease has progressed to more advanced stages, treatment usually involves periodontal surgery. Periodontal surgery is performed in order to reach deep under the gums and between the teeth in order to remove bacteria and restore healthy gums.
Why are we the best dentists in NYC for periodontal disease?
At Sachar Dental NYC, we have a periodontal specialist on our team and in our office. He adheres to our philosophy of performing the most conservative, and least invasive treatment options available. We do not rush into periodontal surgery when less invasive forms of treatment may be able to treat periodontal disease. When periodontal surgery is indicated for more advanced periodontal disease, we are experts in this type of treatment.
Our philosophy is also strongly based on prevention of periodontal disease as the best treatment option. Catching periodontal disease in the early stages allows us to treat it successfully, often with less invasive techniques. We strongly believe in keeping to an extract and regular schedule of dental checkups and professional dental cleanings in order to prevent periodontal disease. Our dental hygienists have advanced training and understanding of periodontal disease, and they are experts in preventing it. They are highly skilled in performing regular dental cleanings in order to prevent periodontal disease before it even starts, and deep cleanings to treat it in its early stages.


